|
Aseptic Necrosis (Avascular Necrosis or Osteonecrosis) What is aseptic necrosis? Aseptic necrosis (also referred to as avascular necrosis or osteonecrosis) is a condition that results from poor blood supply to an area of bone causing bone death. This is a serious condition because the dead areas of bone do not function normally, are weakened, and can collapse. What causes aseptic necrosis? Aseptic necrosis can be caused by trauma and damage to the blood vessels that supply bone its oxygen. Other causes of poor blood circulation to the bone include an embolism of air or fat that blocks the blood flow through the blood vessels, abnormally thick blood (hypercoaguable state), and inflammation of the blood vessel walls (vasculitis). What conditions are associated with aseptic necrosis? Conditions that are associated with aseptic necrosis include alcoholism, steroid usage, Cushing's syndrome, radiation exposure, sickle cell disease, pancreatitis, Gaucher's disease, and systemic lupus erythematosus. How is aseptic necrosis diagnosed? The diagnosis of aseptic necrosis can be made with x-rays, but this is a later stage finding. Earlier signs of avascular necrosis can be detected with MRI scanning or suggested by nuclear bone scanning. What is the treatment for aseptic necrosis? The treatment of aseptic necrosis is critically dependent on the stage of the condition. Early aseptic necrosis (before x-ray changes are evident) can be treated with a surgical operation called a core decompression. This procedure involves removing a core of bone from the involved area and sometimes grafting new bone into the area. This allows new blood supply to form, preserving the bone. Weight bearing should be restricted. Later stages of aseptic necrosis (when x-ray changes have occurred) inevitably lead to seriously damaged bone and joints requiring joint replacement surgery.
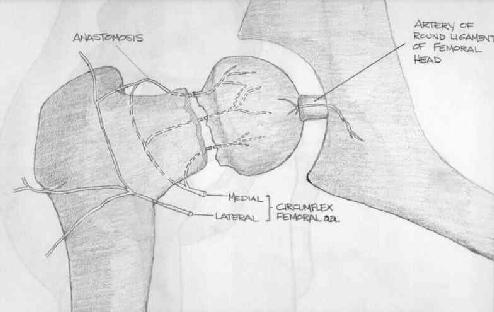
Certain particular bony areas are prone to development of osteonecrosis because of their relatively precarious blood suply
Avascular necrosis occurs in other bones, particulary: -Humeral head -Femoral condiles -Tibial plateau -Talus -Lunate -Scafoid Patogenesis:-Infarction causes marrow edema and venous outflow obstruction, increasing pressure and widening the area of infarction. -Hiperemia of the sorrounding bones causes osteoporosis of living bone,while infarcted bone retains its density and thus appears whiter or denser on roentgenogram. -The bone is gradually revascularized. But bone reabsortion can lead to mecanical failure, with subcondral fractures (crescent sign). -the result is flattening of femoral head, whith incongruity of joint and rapidy progression of secondary osteoarthritis. Clinical manifestations:-Hip pain, particulary with weigth bearing and rotation. -limitation of wiegth bearing and motion. Radiographs:-Can be normal initially,but frequently shows increased density of necrotic bone. -Conbination of osteoclastic and new bone formation in revascularized areas creates x-ray appearance of mottled density. -When collapse of segment of necrotic bone occurs, the compression more bone into smaller area also produces increased x-ray density. -Evaluation includes and AP view and frog-leg lateral x-rays of hip. Bone scanning:-Often shows increased uptake around the necrotic bone.This represents acumulation of radionuclide in the area of increased bone turnover, at the junction beetwen dead and reactive bone. Magnetic ressonance imaging:-Prefered method for differential diagnosis and for radiollogically occult necrosis, since its more sensitive than bone scans or plain films.
-also used to outline the area of involvement. Differential diagnosis:-Sinovitis -Transient osteoporosis -Femoral neck stress fractures -Metastatic diseases
Classification (Enneking`s stages of osteonecrosis):
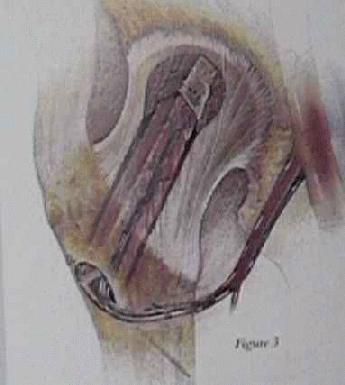
Treatment: Stages I, II, and III:-Core decompression - Wherin a channel is drilled throught the femoral neck.This procedure does give good relief. But this procedure is very controversial, because subsequent series have had failed.
Free vacularized fibular grafting
Treatment: Stages IV and V:-Total hip arthroplasty - Ongoing concern over cement disease, particulate matter, and stress shield changes in the femur inthe cemented or non cemented protheses makes a total hip arthroplasty a less desirably option. Can, also be tried for stage VI. -Bipolar arthroplasty - Worst results are found, probably because of use of thin polyethylene in young heathy patients. -Arthrodesis - Poor choice for bilateral necrosis (50 - 80%) Biblioghraphy:Mankin HJ: Non traumatic necrosis of bone (osteonecrosis). N Engl J Med 1992;326:1473
For related information, please visit the Total Hip Replacement and Total Knee Replacement forums. For further information, please visit the following site: |
Information provided by MedicineNet Used here with permission